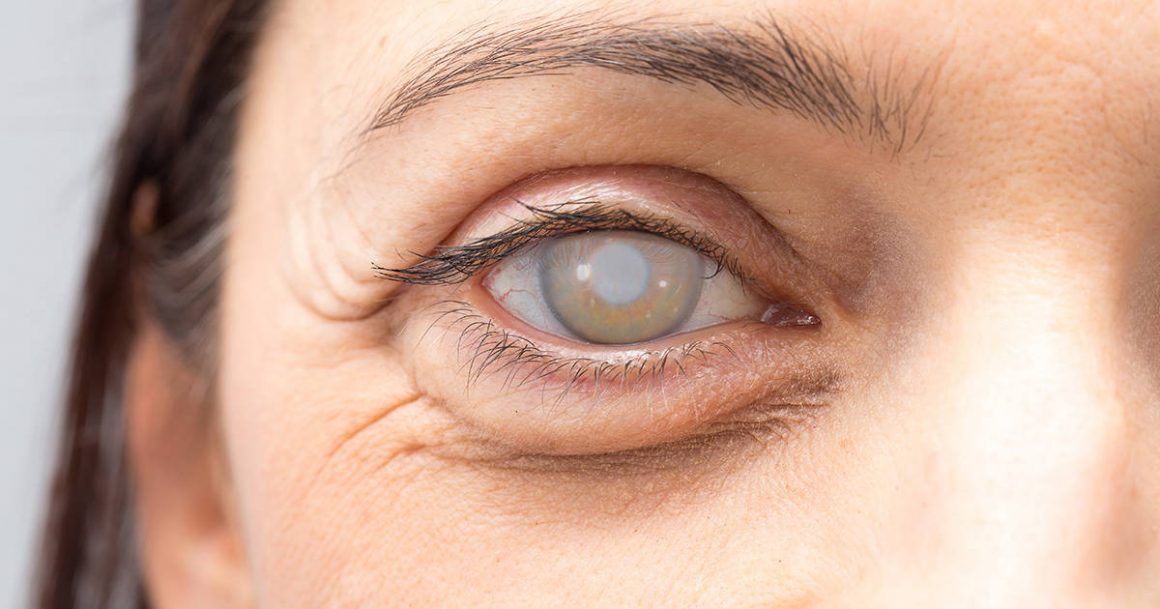
Definition and causes:
In the eye there is a lens that is behind the iris and is called “Crystalline”, this lens has the ability to change its thickness and thus acquire more power to focus and this helps us see objects close. With the passage of time, the Crystalline begins to become opaque and hard and that we call “Cataract”, this situation is normal and will happen to all of us, occurs more quickly in patients with diabetes or other metabolic disease, rheumatoid arthritis and other inflammatory diseases, as well as those who use steroids for long periods.


Symptoms:
- Blurred vision, mainly in the afternoon/evening
- Discomfort with intense light
- Colors become opaque
- Changes in graduation
- They require more light to do their activities since the entrance of light to the eye decreases
- Vision of halos around lights
- Double vision in one eye (very rare)
- In some patients, near vision may improve and they begin to read without glasses.
As the cataract progresses, the symptoms become more severe and if left untreated, can lead to blindness.
Risk factors:
- Age
- Diabetes and other metabolic diseases
- Inflammatory and autoimmune diseases
- Previous eye surgeries
- Smoking
- Long-term use of Cortisone
- UV exposure
- Trauma


Diagnosis:
It is done during a consultation with the Ophthalmologist and the review in the Slit Lamp with the pupil dilated. Visual acuity is measured with and without lenses and intraocular pressure, as well as the fundus of the eye in patients with non-advanced cataracts.
An important point is to measure the amount of Astigmatism that the patient presents, since it is of vital importance at the moment of deciding which intraocular lens to implant.
The first consultation lasts almost an hour since it is necessary to wait until the pupil dilates to conclude the review, the drops cause a dilation of six hours so it is convenient that the patient comes with a companion and has no major events scheduled after the review.
It is not necessary to remain in absolute rest, you can go out, watch TV, there are no limitations in the diet, but those already imposed by some condition such as Diabetes Mellitus, it is normal to feel some discomfort, burning and itching, these symptoms should decrease in the following hours and with the application of the drops.
Intraocular Lens Options
During cataract surgery, the lens with which we are born “crystalline” and which allows us to focus on close objects is being removed, so we must replace it with an artificial lens. There are a wide variety of options and commercial houses, but we can reduce them to four types depending on the distances of vision they correct. All intraocular lenses have UV filters and last a lifetime so they do not require replacement over time.
+ Monofocal: It has graduation for only one distance, far vision is very good without glasses, but they require graduation for intermediate and near vision, there are usually no halos or lights and no adaptation period is required.
+ Monofocal Toric: It has graduation for a single distance, but also corrects the astigmatism that the patient has, requires a special marking in the eye before surgery, this marking is simple, fast and painless. Distance vision is very good without the need for glasses, but they need glasses for intermediate and near vision. There are usually no halos or lights and no adaptation period is required.
+ Trifocal: It is a special lens that has different graduation for different distances, so it allows good vision both distant and intermediate and close. This lens requires good lighting to work well, it achieves a lens independence of up to 95%. It requires an adaptation period and may present halos around the lights, especially at night because in the dark the pupil dilates and the first rings are exposed, so when the light passes through the edge of the ring it is slightly diffused. In the patients in which it appears, most of them stop noticing it after a few weeks. It requires an adaptation period of between two and three weeks.
+ Toric Trifocal: It has the same characteristics as the Trifocal but it also corrects the patient’s Astigmatism so it does not require frame lenses to have the best possible vision.

The risks of surgery are:
+ Corneal Decompensation: More frequent in older patients, diabetics, history of multiple surgeries or with previous corneal alterations, it is treated with anti-inflammatory and hyperosmotic drops. In few cases it can lead to the need of a corneal transplant as a definitive treatment.
+ Severe inflammation during surgery that prevents placement of the intraocular lens: which cannot be foreseen and forces the surgeon to implant the intraocular lens in a second procedure, once the inflammation has subsided, which is treated with drops, ointments and anti-inflammatory intraocular injections.
+ Cystic Macular Edema: in some patients the accumulation of fluid in a part of the eye called the macula can occur due to inflammation which should be treated with injections of steroidal anti-inflammatory outside the eye and with anti-inflammatory drops.
+ Rupture of the posterior lens capsule: which can generate more inflammation and the need to implant the intraocular lens in a second surgery.
+ Severe postoperative inflammation: in some cases there is a greater inflammation than common, in most patients is due to greater response to some component of the materials or consumables used during surgery, treatment is by anti-inflammatory drugs derived from Cortisone for prolonged periods, in some cases up to two or three months.
+ Intracular Infection “Endophthalmitis”: In most cases the associated microorganism is found in the patient’s ocular surface, the way to reduce this risk is by applying topical antibiotic drops prior to surgery, using sterile material, instruments, consumables and intraocular lens and is treated with immediate topical antibiotics and anti-inflammatory and injected intraocularly. Sometimes it requires a Vitrectomy.
+ Retinal Detachment: that the risk can be reduced by performing a good previous revision with the dilated pupil and which is treated with the application of intraocular gas or surgery
+ Choroidal Bleeding “Expulsive Bleeding”: Which cannot be predicted and when it happens the eye must be closed immediately and anti-inflammatory steroids initiated, it is a severe complication that can cause total loss of function.
+ Periocular Hemorrhage: in case of total cataract, the technique used is the extraocular extraction of the complete cataract and requires the application of an injection of anesthesia outside the eye which can result in periocular hemorrhage that causes the suspension of the surgery in which the hemorrhage is resolved.
Rear Capsule Opacity
As we had explained before, during surgery, the cataract is separated from its bag and then removed, and the bag is used as a place to place the implanted intraocular lens. There are always cells left in the bag that can migrate to the posterior capsule, proliferate and form an opacity. This happens in approximately 40% of patients and occurs months or years after surgery. There are those who call it a secondary cataract.
The patient begins to notice that his vision is decreasing again, the light disturbs a lot and the colors are no longer so clear
Technology has helped us to reduce their presentation since we can aspirate more epithelial cells at the end of the surgery and the implanted lenses have square edges that adhere better to the periphery of the capsule and serve as a barrier to the passage of the cells.
It is treated with special laser shots called Nd:YAG, the procedure is very fast, simple and painless, it is performed in the office under pupil dilation and the effect on vision is noticed once pupil dilation is over.